Post-ICU Syndrome and the Importance of Humanization in Intensive Care
Irma Marisol Quiroga-Mantilla 1, Cecilia Teresita De Jesús Carbajal-Llauce 2, Leonor Concepción Vera-Macias3, María Fernanda Calderón-León4, Jorge Eduardo Bejarano-Macias5,
Javier Aquiles Hidalgo- Acosta6*
Javier Aquiles Hidalgo- Acosta6*
1Universidad Cesar Vallejo / Trujillo/ La Libertad/ Perú; irmaquiroga61@gmail.com.
2Universidad Cesar Vallejo / Trujillo/ La Libertad/ Perú; cllaucect@ucvvirtual.edu.pe.
3Universidad de Guayaquil / Ecuador; Leonor.veram@ug.edu.ec.
4Hospital Universitario de Guayaquil / Ecuador; dracalderonleon@hotmail.es.
5Universidad Católica de Santiago de Guayaquil / Ecuador; cirugiacapilar@drpelo.org
6Universidad Espíritu Santo UEES / Guayaquil / Ecuador;
* Correspondence: e-mail: jahidalgoacosta@hotmail.com; Tel.: +593990733946
* Correspondence: e-mail: jahidalgoacosta@hotmail.com; Tel.: +593990733946
Humanization in the ICU has become a central topic over the last decade. New research focuses on technologies such as virtual reality and music therapy, as well as on practices like family presence during and after ICU stays, open-door policies, and monitoring of both family members and healthcare personnel. Psychiatric disorders, including depression, post-traumatic stress, anxiety, and delirium, are prevalent in ICU survivors and contribute to post-ICU syndrome. This research aimed to determine the role of humanization in critical care, with a secondary objective of evaluating the impact of open-door policies on critically ill patients. Analyses, results tables, and conclusions are presented. Humanization encompasses improvements and new associated concepts such as end-of-life care, personalized ICU-VIP care, and virtual reality in the ICU. Flexibility is crucial to address all factors that affect long-term neuropsychiatric outcomes. Humanizing the intensive care unit improves communication and information flow, ultimately reducing delirium and neuropsychiatric symptoms.
Keywords: Humanism; Humanities; Intensive Care; Neonatal Intensive Care; Telecare; Tele-Intensive Care.
INTRODUCTION
This Short Review examines interventions for humanization in the ICU for adult patients, focusing on family presence and effective communication. Studies evaluating the impact of these interventions on reducing post-ICU syndrome and improving patient satisfaction are reviewed. Studies conducted in different contexts, including the COVID-19 pandemic, are included.
Humanization in the intensive care unit refers to the application of new strategies to improve the care of critically ill patients in both their physical and emotional aspects. This research is justified as a topic of great importance that leads to a literature review. 1
Post-Intensive Care Syndrome (PICS)
Patients admitted to the intensive care area generally suffer from disorders that can persist for prolonged periods and that affect their functional capacity and quality of life; in other cases, there are consequences such as post-intensive care syndrome (post-ICU), known as sequelae in critical patients who exceed the stay in the ICU, developing pathological states such as depression, anxiety, delirium and various psychiatric disorders, which will influence their quality of life, which is why the implementation of the humanization of intensive care wards is encouraged, to reduce all these adverse effects or at least in their vast majority. 2
Therapies to Improve Hospital Quality
The application of various therapies that improve hospital quality is proposed for both the patient and the family. It focuses on preventing and rehabilitating mental and cognitive affectations, generating a potential benefit to reduce the sequelae of prolonged stay in the ICU. Research is currently being carried out on the anxiolytic properties of music and its benefits in the intensive care unit (ICU). 3 It has been observed that neuro-ICU patients recovered from neurological pathologies in the intensive care unit are subjected to emotional distress, so it is necessary to apply measures to reduce emotional stress, which would benefit not only the patient but also their family. 4
Open-Door Policy in ICU
The benefit of access to more extended visits in the intensive care unit (ICU) is an issue of great importance. "Open doors" refers to allowing access to family members or companions at all times during the ICU stay without strict visiting hours. 5 The implementation of the rules of family participation in all aspects is supported as an initiative to incorporate technological standards in ICU, 6 in acute wards or psychiatric ICUs, because multiple disadvantages have been noted for patients hospitalized in closed rooms where family members cannot go, as in countries such as Ecuador where most hospitals do not allow prolonged access in the areas Low self-esteem, low autonomy, feelings of being excluded, confined, and stigmatized are also associated with lower satisfaction with services and higher rates of medication refusal. 7
The open-door ICU includes measures such as intensive staff training in tension reduction techniques, non-violent communication, revision, liberalization of ward rules, opening break rooms, and access to a safe garden. 8
Depression in Sepsis Survivors
Patients with sepsis recovered from the ICU present depression during and after their admission to critical care, so the prevention levels to try to improve these complications in addition to pain include the accompaniment of a family member, 9 because patients with prolonged hospital stays are exposed to a subjective deterioration of mental and functional health. 10
Support Interventions in Pediatric ICUs
The significance of support interventions within pediatric intensive care units (PICUs) is paramount. These interventions encompass a range of strategies designed to provide emotional, social, and practical support to critically ill children and their families.
One crucial aspect of support interventions is facilitating parental involvement in the care of their child. This can include encouraging parents to participate in bedside care, decision-making, and comfort measures. Research has shown that active parental involvement can improve children's outcomes, including reduced anxiety, shorter hospital stays, and enhanced parental satisfaction.
Another vital component is the provision of psychosocial support to families. This can involve connecting families with support groups, providing access to mental health professionals, and offering education about PICU procedures and everyday challenges. By addressing the emotional and psychological needs of families, support interventions can help mitigate the trauma and stress associated with a child's critical illness.
Furthermore, support interventions may also focus on creating a child-friendly and developmentally appropriate environment within the PICU. This can involve incorporating play therapy, providing access to age-appropriate activities, and ensuring a comfortable and welcoming atmosphere. By considering the unique needs of children, support interventions can help promote their well-being and facilitate a smoother recovery process. 11
Flexible Protocols for Critically Ill Patients
Flexible protocols ensure that critically ill patients receive individualized care that meets their unique needs and preferences. These protocols prioritize patient autonomy and comfort by allowing adaptability in visitation policies, treatment plans, and daily routines.
One example of flexible protocols is open visitation policies, which allow patients to remain accompanied by their chosen family members or support persons for extended periods, often without strict time restrictions. This can help alleviate feelings of isolation and anxiety for patients and provide them with much-needed emotional support during their critical illness.
Flexible protocols can also extend to treatment plans, allowing for adjustments based on patient response and preferences. This can involve incorporating complementary therapies, such as music therapy or aromatherapy, to address pain and anxiety. Additionally, flexible protocols can promote patient comfort by allowing personalized daily routines, such as adjusting meal times or providing opportunities for rest.
By adopting flexible protocols, intensive care units can create a more patient-centered environment that prioritizes individual needs and preferences. This approach can improve patient satisfaction, reduce stress, and enhance overall well-being during a challenging time.
Humanization in the ICU
Humanization arises from the need to improve the experience during and after admission to the ICU for the patient, the family, and the health personnel; several factors contribute to dehumanizing the ICU; among the most critical factors are the restricted visiting schedules that keep the family member away from contact with the patient, the environmental discomfort caused by noise, The lights that are generated in the intensive care unit prevent patients from sleeping, all of which are factors that can be improved by treating family members and the patient with empathy. 13
Communication Barriers in the ICU
An essential factor refers to the communication of patients who are admitted to the ICU, sometimes they are recovering from the effect of sedatives and neuromuscular relaxants, they remain intubated connected to mechanical ventilation, weaning is performed with an awake patient, sometimes intubated or extubated, so it is difficult to communicate, which is one of the main barriers that affects humanization in the ICU, Lack of communication can be associated with physical and psychological damage from not being able to express their emotions. 14
Patient- and Family-Centered Care
Patient- and family-centered care (PFCC) is a healthcare approach that prioritizes the active involvement of patients and their families in all aspects of care. It is based on the belief that patients and families are partners in the healthcare process and that their perspectives, values, and preferences should be respected and incorporated into treatment decisions.
In the context of intensive care, PFCC is particularly important due to the high-stakes nature of critical illness and the potential for significant emotional and psychological distress for both patients and families. By adopting a PFCC approach, intensive care units can create a more supportive and collaborative environment that fosters trust, communication and shared decision-making.
Critical elements of PFCC in the ICU include:
- Open communication: Establishing open and honest communication channels between healthcare providers, patients, and families.
- Respect for preferences: Incorporating patient and family values, preferences, and cultural beliefs into care plans.
- Family presence: Encouraging family presence and participation in patient care and decision-making.
- Shared decision-making: Facilitating shared decision-making between healthcare providers, patients, and families regarding treatment options and goals of care.
- Emotional support: Providing emotional support to patients and families, including access to mental health professionals and support groups.
By embracing PFCC, intensive care units can promote a more humanized and compassionate environment that prioritizes the holistic needs of patients and their families. This approach can improve patient satisfaction, reduce stress, and enhance overall well-being during a critical illness.
Post-ICU Syndrome
Post-ICU syndrome occurs in more than half of adult patients; in children, the syndrome is known as pediatric post-intensive care syndrome (PICS-p); after discharge from the ICU its presentation can cause physical deficits, psychological disorders, cognitive impairment, social disorders to adapt after medical discharge make it necessary to have a humanized care perspective with quality and warmth. 16
Humanized ICU Care Model
A model based on humanized ICU care that focuses on all aspects, such as avoiding all the above factors, will help improve care. 17
New Technologies in the ICU During the COVID-19 Pandemic
During the COVID-19 pandemic, visits to patients and the accompaniment of family members in intensive care wards were reduced due to the spread of the virus or confinement; new technologies were implemented in 96.5% of the 57 Spanish ICUs surveyed during the pandemic, the vast majority-maintained humanization with good communication between the patient, family member, and doctor virtually. 18 Evaluating and providing feedback is necessary to carry out humanized patient care in the public sphere. A study revealed that humanism, quality, safety, learning, support assistance, and help for patients, families, and health personnel are needed for humanization. 19 Humanization is an integral part of the manual of good practices in ICU that includes humanization at any point in the hospital, such as the ICU, resuscitation, or any critical patient care unit, marked as the first line to humanize the ICU with open doors, participation of the family member in care, secondly, Communication in the team, communication of information to family members with communication to the patient. Improve the patient's physical, psychological, autonomy, and adequate environment with hours of rest at night, in addition to care for professionals, follow-up of the post-ICU syndrome, end-of-life care, and guaranteed humanized infrastructure. 20 post-ICU syndrome (PICS), research on PICS shows that in severe cases such as respiratory distress, in most cases, intubated patients are on invasive mechanical ventilation or non-invasive mechanical ventilation, need for central venous catheters, catheters, and other devices the study observed that during the pandemic 9 out of 10 surviving patients presented PICS in pneumonia due to COVID 19 this infection of the SARS Cov 2. 21
Preventing PICS
Future directions are aimed at preventing this psychiatric syndrome with the humanization of the patient and the family so that the disease can pass in the intensive care unit. This is a concept applied to adults and pediatric patients; the PICS-F refers to the psychiatric disorder that affects 22 research such as psychoeducation to the family to prevent PICS through smartphone applications belong to the recent advances include follow-up of the family member even after discharge, and was shown to have good results in patients who underwent telephone intervention, fewer PICS disorders. 23
Music therapy in the intensive care unit is a novel measure of recent years, which improves delirium in critically ill patients, evidenced in a randomized study carried out in 36 patients that showed that music therapy decreases delirium and the number of days on mechanical ventilation, providing a result of great importance for the management of patients who are under sedation or in the process of weaning (p < 0.05). 24
An improvement in quality of life is observed in surviving ICU patients after applying dyadic resilience, which refers to the equal and joint treatment of the patient and their family members. A study showed that patients significantly improved their physical and environmental quality of life, overall quality of life, and satisfaction when they provided accompaniment and dyadic resilience with their family members. 25
Virtual reality in the ICU (ICU-VR) consists of a 14-minute informative video that can be watched through virtual reality in the intervention of the patient in the ICU environment, received explanations about different roles of the ICU and treatment; this randomized study revealed that the implementation of this technology is possible in the field of critical care, including patients with COVID 19, being an innovative feasible and acceptable method to improve satisfaction. 26
Issues arise from end-of-life care, such as the care of patients as significant persons (VIPs) before their admission to the ICU. In this regard, in a study carried out in the western region of China in patients with advanced tumors, the result was that after 1 month of intervention with VIP care, poor quality of life, physical discomfort, and negative emotions improved, obtaining favorable results and changes for the patient. 27
Psychiatric wards with open doors increasingly question the need for closed units in psychiatric hospitals, emergency rooms, and intensive care. 28
Tables 1, 2, and 3 show the results on the benefits, challenges, limitations, and implementation of open-door ICU policies with results from a balanced perspective in Figure 1 panel (a) ICU with natural light, panel (b) the monitor with heart rhythm alteration generates annoying noises to patients and panel c critical patient in the operating room all the environment that surrounds the patient is observed. A seriously ill patient is seen in an image of an acute operating room, panel c critical patient in the ICU room undergoing an invasive procedure for which total analgesia is necessary.
Table 1 PICS and its management in the ICU summarize the PICS management and the patient's characteristics.
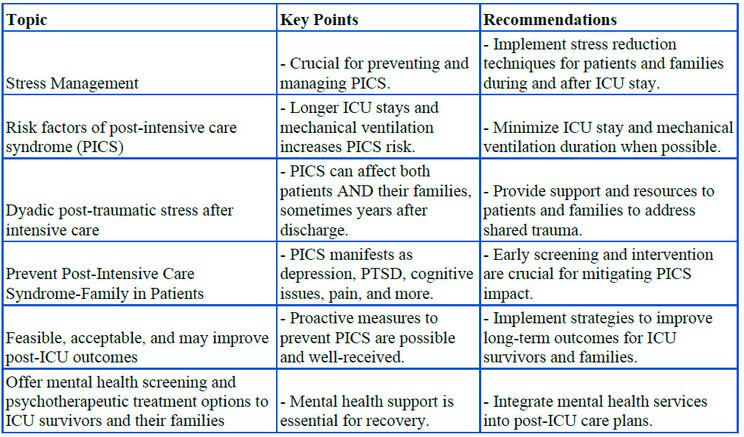
Table 1. PICS in patients with post-ICU recovery. Summarizes the management of PICS and the characteristics of the patients. 29, 30, 31
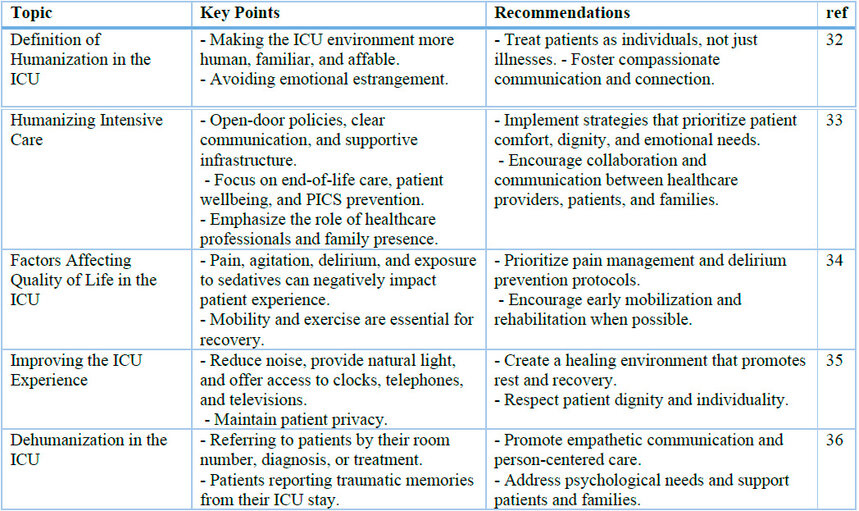
Table 2. This table discusses the ethical implications and characteristics of humanization in UCI. Characteristic's humanization
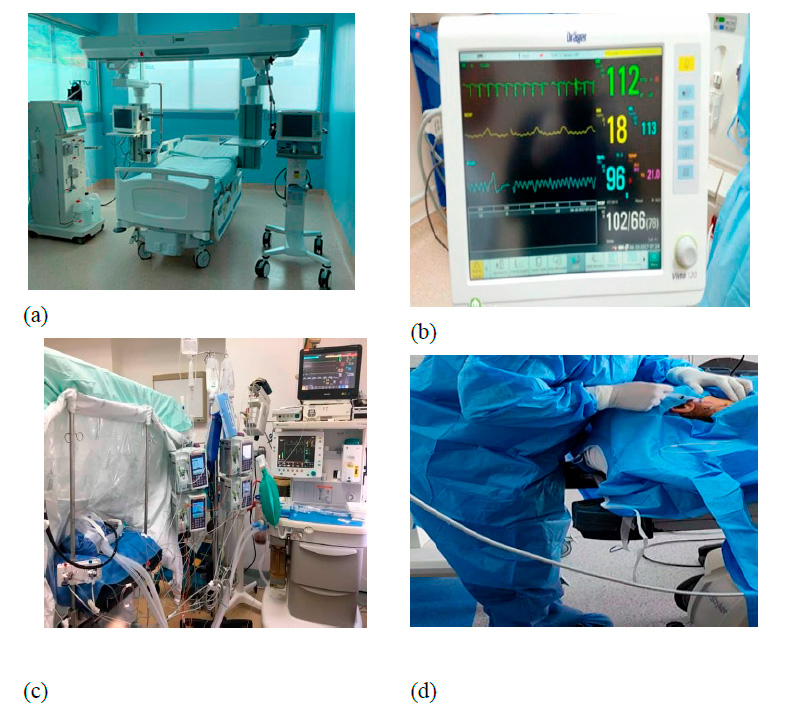
Figure 1. (a) the panel shows an ICU bed, mechanical ventilator, hemodialysis machine, monitors, and natural light during the day; (b) the panel contains a monitor with tachycardia in the ICU. Humanization aims to reduce all this burden on the patient and the family. In panels c and d, critically ill patients are sometimes undergoing procedures that can cause pain, anxiety, or stress.
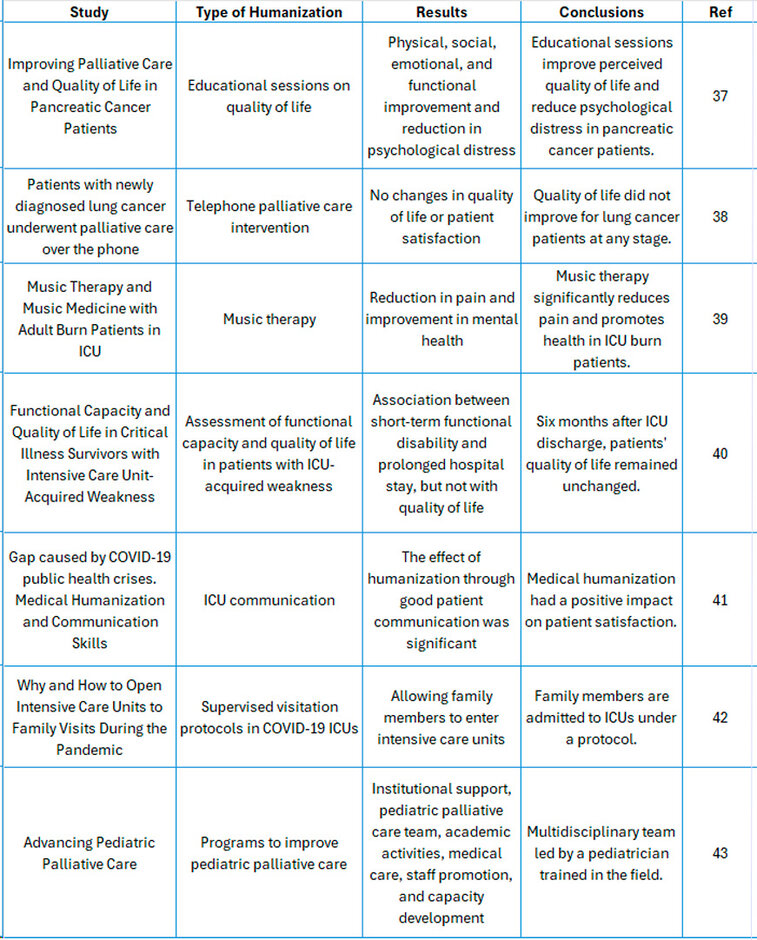
Table 3. Humanizacion in UCI Paradigms.
Bu et al. (2024) investigated the impact of medical humanization and communication skills on patient satisfaction during the COVID-19 pandemic. The authors argue that public health crises like the pandemic can exacerbate feelings of dehumanization and isolation among patients, highlighting the need for healthcare providers to prioritize compassionate communication and patient-centered care. The study examined the relationship between medical humanization, communication, patient satisfaction, and the moderating role of trust in medical institutions.
The findings revealed that effective communication is crucial in mediating the relationship between medical humanization and patient satisfaction. In other words, when healthcare providers communicate effectively and demonstrate empathy, patients are more likely to feel valued and understood, leading to greater satisfaction with their care. Furthermore, the study found that trust in medical institutions strengthens this relationship, suggesting that patients who trust their healthcare providers are more likely to benefit from humanized care and effective communication.
This research underscores the importance of humanization and communication in healthcare, particularly during times of crisis. By fostering a sense of connection and trust, healthcare providers can help patients cope with illness and uncertainty, ultimately improving their overall experience and well-being.41
The COVID-19 pandemic brought about unprecedented restrictions on family presence in intensive care units (ICUs) worldwide. The article "Why and how to open intensive care units to family visits during the pandemic" by Mistraletti et al. (2021) argues for the importance of reinstating family visits in ICUs, " and provides recommendations for safe visitation protocols. The authors highlight the numerous benefits of family presence for patients and their families, such as reduced anxiety and delirium, shorter hospital stays, and improved communication with healthcare providers. They acknowledge the infection control challenges posed by the pandemic but emphasize that these can be mitigated through carefully designed visitation protocols.
The article proposes several measures to ensure safe visitation practices, including limiting the number of visitors, requiring personal protective equipment (PPE), and implementing screening procedures for visitors. Notably, the authors stress the need for flexibility and adaptability in visitation policies, recognizing that local circumstances and the evolving epidemiological situation may require protocol adjustments. They advocate for a balanced approach that prioritizes patient safety and the psychosocial wellbeing of patients and families. In conclusion, Mistraletti et al. make a compelling case for the importance of family presence in the ICU and offer practical guidance for implementing safe visitation protocols during a pandemic. By striking a balance between infection control and compassionate care, hospitals can ensure that critically ill patients receive the support they need from their loved ones while minimizing the risk of viral transmission.42
A study conducted in Italy in pediatric ICUs in seven centers investigated humanization in critical areas; humanization questionnaires indicated a lack of recreational facilities, mediation, and translation services. 44 In Italian ICUs during the lockdown, 11,102 adult patients were admitted to ICUs, 6% of patients received at least one visit. 45
A study in Romania revealed greater empathy in nurses who carried out their work at the community level and demonstrated high levels of empathy with low-stress levels. 46
Restricted visitation policies must be carried out in strictly necessary cases; a great example was lung infection caused by SARS Cov 2, one of the containment measures of the virus included doors of restricted visits in ICUs; these measures that were implemented during the pandemic increased the burden in all aspects to the health system. 47
Communication and visits need to be more face-to-face for patients with end-of-life care; for this reason, these measures must be implemented in all aspects. 48
Most research focuses on humanization, sensitivity, and ethics, which must be a guarantee in the intensive care unit and a good level of satisfaction. 49, 50
Currently, technology in intensive care areas allows a better communication interface in patients connected to mechanical ventilation who have difficulty communicating, and eye-tracking devices serve as tools to allow better doctor-patient communication. 51
A randomized controlled trial showed that family visits in the ICU can help reduce stress by improving parameters in the heart rate. 52
Negative results in open-door ICUs were presented in a low percentage in psychiatric wards, where violence by patients towards medical personnel was one of the main problems, generating leakage mainly in acute psychiatric wards, which required many health personnel and costs to be able to apply humanization. 53, 54
The studies that resulted with a favorable effect concluded that music therapy reduces delirium and that virtual reality improves care in the ICU, providing a better quality of life from admission, with better stress management. 55
Music therapy or aromatherapy in burn patients is favorable because it reduces pain and anxiety and increases relaxation. 56
In the health crisis caused by COVID-19, patients positively correlated humanization with good communication and implementation of technology with communication interfaces between doctors and mechanically ventilated patients, reaching statistical significance, demonstrating that visits in open-door ICUs improve the heart rate of hospitalized patients; however, satisfaction with humanization did not improve significantly in care palliative care by telephone, for cancer patients, in different stages, did not improve either, in support of a navigator for parents, to whom intervention was performed, not achieving statistical significance. 57
Limitations of the evidence depend on the feasibility of the evaluation; for example, in situations such as sleep, there is some difficulty in performing an electroencephalogram to evaluate sleep with music therapy, which is part of the humanization in the ICU, being unfeasible due to the effects it caused in the patient (movements), altering the correct performance of the exam. This results in high costs and economic factors due to the mobilization of medical instruments and personnel. 58
Critical analysis of evidence from clinical trials and meta-analyses that reported the statistical value of humanization in ICU. Statistical significance P value
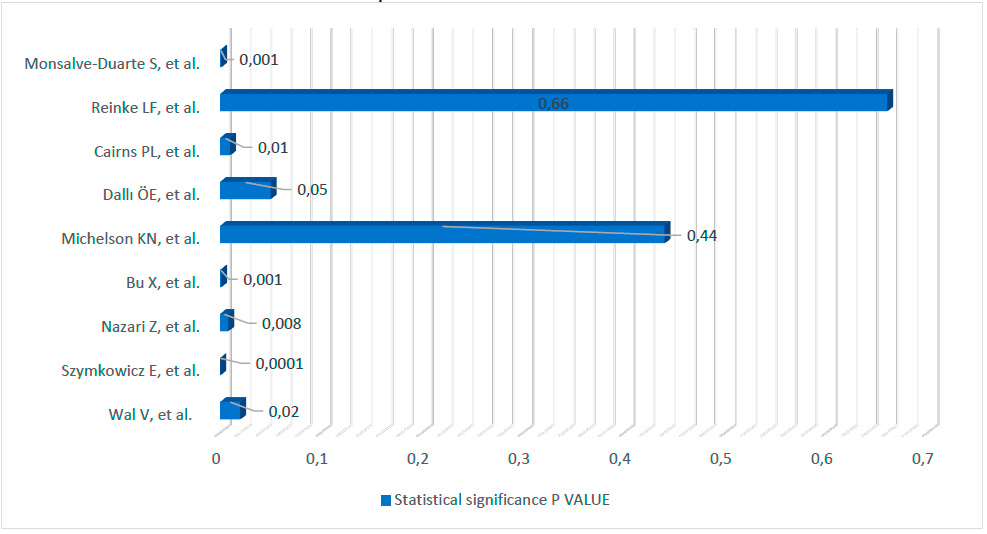
Figure 2. Evidence from clinical trials and meta-analyses reported humanization's statistical value in ICUs.
Certainty of evidence to perform the final analysis, studies with scientific relevance were compared, and clinical tests and high-quality meta-analyses were used from randomized studies, which compared different forms of humanization; no significant differences were found in long-term or short-term mortality. The statistical benefit was based on simple applications to improve sleep, reduce noise, flexibility of visits to family members, and patient satisfaction, which helped significantly reduce stress in the patient.
Assessing evidence bias
The heterogeneity of the recruited population provided differences in the characteristics of the studied patients admitted to the ICU; for example, patients with better quality of life before admission to the ICU had better responses in the evaluation of their perspectives of deferred consent, unlike patients evaluated with worse quality of life, did not remember their participation and had even hostile responses. Different interventions in humanization were observed. The differences in the technological tools evaluated in the research varied greatly and generated statistical heterogeneity ( Figure 2).
Benefits in the perception of the mother in the neonatal intensive care unit: mothers felt satisfaction in staying with the newborn, helping in the care of the child, improving the maternal bond, and constantly observing the evolution, in addition to showing the quality of intensive care, 59 the neonatal ICU is a highly stressful environment, for this reason, it is necessary to take emotional care of the families, the open doors favor the mother-child bond. 60
Several events in the ICU environment can be improved through the presence of family, a welcoming relationship, and sensitive intensive care staff. 61
During the pandemic, the quality of life of cancer patients was affected, the proximity of patients admitted to the ICU was affected, patients were affected, and the exclusion of essential people in end-of-life care; for this reason, it is necessary to improve all aspects of humanization. 62, 63
Patients who are admitted to the ICU need to recover psychologically from negative psychological situations that are represented during their stay in the intensive care unit and thus be able to manage the post-ICU syndrome adequately. 64
Future research on humanization must be focused on the development of an environment as effectively as possible; research on new technologies such as virtual reality, mixed reality, simulation, and artificial intelligence could improve these aspects that are still unknown; the present review considers it necessary to do more high-quality research that evaluates each situation that can improve the care of critical patients in the future. to avoid all complications related to the psychology of the patient admitted to critical care and their family.
CONCLUSIONS
Humanization in the ICU offers diverse strategies to enhance patients' and their families' capacity to cope with and overcome the challenges inherent to critical illness and intensive care. This review has highlighted the multifaceted nature of humanization, encompassing interventions such as family presence, effective communication, technology utilization, and environmental modifications.
The evidence presented underscores the positive impact of humanization on patient outcomes, including reduced delirium, anxiety, post-ICU syndrome, and improved patient satisfaction and overall well-being. Notably, interventions such as music therapy and open visitation policies have shown promising results in mitigating the adverse effects of critical illness and fostering a more supportive and healing environment.
However, the review also acknowledges the challenges and limitations of implementing humanization in the ICU. Factors such as resource constraints, resistance to change, and further research in specific areas require careful consideration and ongoing efforts to address.
Moving forward, it is imperative to continue exploring and refining ICU humanization interventions. Future research should focus on evaluating the long-term effects of humanization, identifying optimal strategies for different patient populations, and developing comprehensive frameworks for implementation in diverse healthcare settings. By prioritizing humanization as a core component of intensive care, we can create a more compassionate and patient-centered environment that promotes healing, well-being, and recovery.
Author Contributions: Conceptualization, J.H. and I.Q; methodology, M.C.; V.L. software; validation, J.B., C.C. and I.Q.; formal analysis C.M.; research, H.J., B.J.; resources, I.Q., V.L., J.B.; H.J. data curation; writing: preparation of the original draft M.C.; writing: proofreading and editing, C.M.; DC display; supervision, J.H, JB.; project management, I.Q.; Acquisition of Funds, C.M. All authors have read and agree with the published version of the manuscript.
Funding: without any external financing.
Institutional Review Board Statement: Not applicable.
Informed Consent Statement: Written informed consent is given for the article's publication.
Acknowledgments: To my mother.
Conflicts of Interest: The authors declare no conflict of interest in this research.
REFERENCES
1.- Soto S, Navarro S, Daniela A, Evidence on prevention and rehabilitation strategies for post-ICU syndrome in adults: a review of systematic reviews, Acta Colombiana de Cuidado Intensivos. Colombian Inten-sive Care Act. 2023; Volume 23: Pages 273-285. https://doi.org/10.1016/j.acci.2023.04.001
2.- Sidiras G, Patsaki I, Karatzanos E, Dakoutrou M, Kouvarakos A, Mitsiou G, Routsi C, Stranjalis G, Nan-as S, Gerovasili V. Long-term follow-up of quality of life and functional ability in patients with ICU ac-quired Weakness - A post hoc analysis. J Crit Care. 2019 Oct;53:223-230. doi: 10.1016/j.jcrc.2019.06.022.
3.- Seyffert S, Moiz S, Coghlan M, Balozian P, Nasser J, Rached EA, Jamil Y, Naqvi K, Rawlings L, Per-kins AJ, Gao S, Hunter JD 3rd, Khan S, Heiderscheit A, Chlan LL, Khan B. Decreasing delirium through music listening (DDM) in critically ill, mechanically ventilated older adults in the intensive care unit: a two-arm, parallel-group, randomized clinical trial. Trials. 2022 Jul 19;23(1):576. doi: 10.1186/s13063-022-06448-w.
4.- Bannon SM, Cornelius T, Gates MV, Lester E, Mace RA, Popok P, Macklin EA, Rosand J, Vranceanu AM. Emotional distress in neuro-ICU survivor-caregiver dyads: The recovering together randomized clinical trial. Health Psychol. 2022 Apr;41(4):268-277. doi: 10.1037/hea0001102.
5.- Milner KA, Marmo S, Goncalves S. Implementation and sustainment strategies for open visitation in the intensive care unit: A multicentre qualitative study. Intensive Crit Care Nurs. 2021 Feb;62:102927. doi: 10.1016/j.iccn.2020.102927.
6.- Wilson C. The socialization of civic participation norms in government: Assessing the effect of the Open Government Partnership on countries' e-participation. Government Information Quarterly. 2020; 37: 4. https://doi.org/10.1016/j.giq.2020.101476.
7.- Gill NS, Parker S, Amos A, Lakeman R, Emeleus M, Brophy L, Kisely S. Opening the doors: Critically examining the locked wards policy for public mental health inpatient units in Queensland Australia. Aust N Z J Psychiatry. 2021 Sep;55(9):844-848. doi: 10.1177/00048674211025619.
8.- Gouzoulis-Mayfrank E, Gairing SK, Krämer T, Förster M, Schmitz-Buhl M. Öffnung einer psychia-trischen Akutstation als komplexe Intervention [Opening up an acute psychiatric ward as a complex inter-vention]. Nervenarzt. 2019 Jul;90(7):709-714. German. doi: 10.1007/s00115-019-0734-2.
9.- Boede M, Gensichen JS, Jackson JC, Eißler F, Lehmann T, Schulz S, Petersen JJ, Wolf FP, Dreischulte T, Schmidt KFR. Trajectories of depression in sepsis survivors: an observational cohort study. Crit Care. 2021 Apr 29;25(1):161. doi: 10.1186/s13054-021-03577-7.
10.- Paul N, Cittadino J, Krampe H, Denke C, Spies CD, Weiss B. Determinants of Subjective Mental and Functional Health of Critical Illness Survivors: Comparing Pre-ICU and Post-ICU Status. Crit Care Med. 2024 May 1;52(5):704-716. doi: 10.1097/CCM.0000000000006158.
11.- Michelson KN, Frader J, Charleston E, Rychlik K, Aniciete DY, Ciolino JD, Sorce LR, Clayman ML, Brown M, Fragen P, Malakooti M, Derrington S, White D; Navigate Study Investigators. A Randomized Comparative Trial to Evaluate a PICU Navigator-Based Parent Support Intervention. Pediatr Crit Care Med. 2020 Sep;21(9):e617-e627. doi: 10.1097/PCC.0000000000002378.
12.- Martínez ZR. Humanization in Intensive Care Unit. Med Crit. 2021; 35(3):144-147. doi:10.35366/100003.
13.- Gareau S, de Oliveira ÉM, Gallani MC. Humanization of care for adult ICU patients: a scoping review protocol. JBI Evid Synth. 2022 Feb; 20(2):647-657. doi: 10.11124/JBIES-20-00481. PMID: 34555837.
14.- Istanboulian L, Rose L, Yunusova Y, Gorospe F, Dale C. Barriers to and facilitators for the use of augmentative and alternative communication and voice restorative devices in the adult intensive care unit: a scoping review protocol. Syst Rev. 2019 Dec 6; 8(1):311. doi: 10.1186/s13643-019-1232-0.
15.- Secunda KE, Kruser JM. Patient-Centered and Family-Centered Care in the Intensive Care Unit. Clin Chest Med. 2022 Sep; 43(3):539-550. doi: 10.1016/j.ccm.2022.05.008.
16.- Yuan C, Timmins F, Thompson DR. Post-intensive care syndrome: A concept analysis. Int J Nurs Stud. 2021 Feb;114:103814. doi: 10.1016/j.ijnurstu.2020.103814.
17.- Tang M, Xu M, Su S, Huang X, Zhang S. Post-Intensive Care Syndrome in Children: A Concept Analysis. J Pediatr Nurs. 2021 Nov-Dec;61:417-423. doi: 10.1016/j.pedn.2021.10.007.
18.- Fernández J, González D, Arroyo J, Garnacho J. National survey on changes in visitation, communica-tion and end-of-life care policies in intensive care units through the different COVID-19 pandemic's waves (COVIFAUCI study). Enfermería Intensiva (edición inglesa). 2024; 35: 35-44. https://doi.org/10.1016/j.enfie.2023.07.004
19.- Vásquez Espinoza G de J, León Samaniego GF, Clavero Soto JC, Encalada Campos GE. Humanized nursing care in the care of patients admitted to public hospitals in the city of Milagro – Ecuador. Medicien-ciasUTA [Internet]. January 1, 2022 [cited May 19, 2024]; 6(1):55-68. Available at: https://revistas.uta.edu.ec/erevista/index.php/medi/article/view/1563.
20.- Martínez ZR. Humanization in the Intensive Care Unit. Med Crit. 2021; 35(3):144-147. doi:10.35366/100003.
21.- Mateo Rodríguez E, Puchades Gimeno F, Ezzeddine Angulo A, Asensio Samper J, Saiz Ruiz C, López Alarcón MD. Postintensive care syndrome in COVID-19. Unicentric pilot study. Med Clin (Barc). 2022 Oct 14;159(7):321-326. English, Spanish. doi: 10.1016/j.medcli.2021.11.014.
22.- Inoue S, Hatakeyama J, Kondo Y, Hifumi T, Sakuramoto H, Kawasaki T, Taito S, Nakamura K, Unoki T, Kawai Y, Kenmotsu Y, Saito M, Yamakawa K, Nishida O. Post-intensive care syndrome: its pathophysi-ology, prevention, and future directions. Acute Med Surg. 2019 Apr 25;6(3):233-246. doi: 10.1002/ams2.415.
23.- Petrinec AB, Wilk C, Hughes JW, Zullo MD, George RL. Self-Care Mental Health App Intervention for Post-Intensive Care Syndrome-Family: A Randomized Pilot Study. Am J Crit Care. 2023 Nov 1;32(6):440-448. doi: 10.4037/ajcc2023800.
24.- Dallı ÖE, Yıldırım Y, Aykar FŞ, Kahveci F. The effect of music on delirium, pain, sedation and anxiety in patients receiving mechanical ventilation in the intensive care unit. Intensive Crit Care Nurs. 2023 Apr;75:103348. doi: 10.1016/j.iccn.2022.103348.
25. - Lester EG, Mace RA, Bannon SM, Popok PJ, Gates MV, Meyers E, Tehan T, Sagueiro D, Rosand J, Macklin EA, Vranceanu AM. Can a Dyadic Resiliency Program Improve Quality of Life in Cognitively In-tact Dyads of Neuro-ICU Survivors and Informal Caregivers? Results from a Pilot RCT. Neurocrit Care. 2021 Dec;35(3):756-766. doi: 10.1007/s12028-021-01222-3.
26.- Vlake JH, van Bommel J, Wils EJ, Bienvenu J, Hellemons ME, Korevaar TI, Schut AF, Labout JA, Schreuder LL, van Bavel MP, Gommers D, van Genderen ME. Intensive Care Unit-Specific Virtual Reality for Critically Ill Patients With COVID-19: Multicenter Randomized Controlled Trial. J Med Internet Res. 2022 Jan 31;24(1):e32368. doi: 10.2196/32368.
27.- Zheng X, Peng Y, Liu C, Li F, Zhang H, Liao J, Wu G, Zeng X, Xie N. Application of VIP Care in Pa-tients with Advanced Tumors in the Western Region of China. Biomed Res Int. 2022 Aug 31;2022:7834620. doi: 10.1155/2022/7834620. Retraction in: Biomed Res Int. 2023 Aug 2;2023:9843473.
28.- Schreiber LK, Metzger FG, Flammer E, Rinke H, Fallgatter AJ, Steinert T. Open Doors by Fair Means: a quasi-experimental controlled study on the effects of an open-door policy on acute psychiatric wards. BMC Health Serv Res. 2022 Jul 22;22(1):941. doi: 10.1186/s12913-022-08322-6.
29.- Cairns PL, Buck HG, Kip KE, Rodriguez CS, Liang Z, Munro CL. Stress Management Intervention to Prevent Post-Intensive Care Syndrome-Family in Patients' Spouses. Am J Crit Care. 2019 Nov;28(6):471-476. doi: 10.4037/ajcc2019668.
30.- Kosilek RP, Schmidt K, Baumeister SE, Gensichen J; SMOOTH Study Group. Frequency and risk fac-tors of post-intensive care syndrome components in a multicenter randomized controlled trial of German sepsis survivors. J Crit Care. 2021 Oct;65:268-273. doi: 10.1016/j.jcrc.2021.07.006.
31.- Gawlytta R, Brunkhorst F, Niemeyer H, Boettche M, Knaevelsrud C, Rosendahl J. Dyadic post-traumatic stress after intensive care: Case report of a sepsis patient and his wife. Intensive Crit Care Nurs. 2020 Jun;58:102806. doi: 10.1016/j.iccn.2020.102806.
32.- Kvande ME, Angel S, Højager Nielsen A. "Humanizing intensive care: A scoping review (HumanIC)". Nurs Ethics. 2022 Mar;29(2):498-510. doi: 10.1177/09697330211050998.
33.- Salazar D, Israel Villalba D, Mendoza J, et al., Humanization of Intensive Care: The Other Side of Medicine. Biomed J Sci & Tech Res 44(2)-2022. BJSTR. MS.ID.007034.
34.- Alonso Á, Heras G. Humanizing care reduces mortality in critically ill patients. Medicina Intensiva (English Edition). March 2020; Volume 44: 122-124. https://doi.org/10.1016/j.medine.2019.03.016.
35.- Latour JM, Kentish-Barnes N, Jacques T, Wysocki M, Azoulay E, Metaxa V. Improving the intensive care experience from the perspectives of different stakeholders. Crit Care. 2022 Jul 18;26(1):218. doi: 10.1186/s13054-022-04094-x.
36.- Wilson, ME, Beesley, S., Grow, A. et al. Humanizar la unidad de cuidados intensivos. Cuidado crítico 23 , 32 (2019). https://doi.org/10.1186/s13054-019-2327-7.
37.- Chung V, Sun V, Ruel N, Smith TJ, Ferrell BR. Improving Palliative Care and Quality of Life in Pan-creatic Cancer Patients. J Palliat Med. 2022 May;25(5):720-727. doi: 10.1089/jpm.2021.0187.
38.- Reinke LF, Sullivan DR, Slatore C, Dransfield MT, Ruedebusch S, Smith P, Rise PJ, Tartaglione EV, Vig EK, Au DH. A Randomized Trial of a Nurse-Led Palliative Care Intervention for Patients with Newly Diagnosed Lung Cancer. J Palliat Med. 2022 Nov;25(11):1668-1676. doi: 10.1089/jpm.2022.0008.
39.- Monsalve-Duarte S, Betancourt-Zapata W, Suarez-Cañon N, Maya R, Salgado-Vasco A, Prieto-Garces S, Marín-Sánchez J, Gómez-Ortega V, Valderrama M, Ettenberger M. Music therapy and music medicine interventions with adult burn patients: A systematic review and meta-analysis. Burns. 2022 May;48(3):510-521. doi: 10.1016/j.burns.2021.11.002.
40.- Eggmann S, Luder G, Verra ML, Irincheeva I, Bastiaenen CHG, Jakob SM. Functional ability and qual-ity of life in critical illness survivors with intensive care unit acquired weakness: A secondary analysis of a randomised controlled trial. PLoS One. 2020 Mar 4;15(3):e0229725. doi: 10.1371/journal.pone.0229725.
41.- Bu, X., Wang, Y., Du, Y. et al. Bridging the gap caused by public health crises: Medical humanization and communication skills build a psychological bond that satisfies patients. Int J Equity Health 2024. 40. https://doi.org/10.1186/s12939-024-02116-4.
42.- Mistraletti, G., Giannini, A., Gristina, G. et al. Why and how to open intensive care units to family visits during the pandemic. Critical Care 25, 191 (2021). https://doi.org/10.1186/s13054-021-03608-3.
43.- García-Quintero, X., Parra-Lara, LG, Claros-Hulbert, A. et al. Advancing Pediatric Palliative Care in a Lower-Middle-Income Country: An Implementation Study, a challenging but not impossible task. BMC Pal-liat Care 19, 170 (2020). https://doi.org/10.1186/s12904-020-00674-2.
44.- Mandate, C., Siano, MA, De Anseris, AGE et al. Humanization of care in paediatric wards: differences between user and staff perceptions according to type of service. Ital J Pediatr 46 , 65 (2020). https://doi.org/10.1186/s13052-020-00824-5.
45.- Langer, T., Depalo, FC, Forlini, C. et al. Communication and visitation policies in Italian intensive care units during the first pandemic wave and COVID-19 lockdown: a nationwide survey. BMC Anesthesiol 22, 187 (2022). https://doi.org/10.1186/s12871-022-01726-1.
46.- Onofrei, L., Serban, CL, Chirita-Emandi, A. et al. The Impact of Theory of Mind, Stress, and Profes-sional Experience on Empathy in Romanian Community Nurses: A Cross-Sectional Study. BMC Nurses 22, 400 (2023). https://doi.org/10.1186/s12912-023-01569-2.
47.- Moss, SJ, Krewulak, KD, Stelfox, HT et al. Políticas de visitas restringidas en entornos de cuidados intensivos durante la pandemia de COVID-19: una revisión del alcance. Cuidado crítico 25 , 347 (2021). https://doi.org/10.1186/s13054-021-03763-7.
48.- Fernández-Castillo RJ, González-Caro MD, Arroyo-Muñoz FJ, Garnacho-Montero J. National survey on changes in visitation, communication and end-of-life care policies in intensive care units through the dif-ferent COVID-19 pandemic's waves (COVIFAUCI study). Enferm Intensiva (Engl Ed). 2024 Jan-Mar;35(1):35-44. doi: 10.1016/j.enfie.2023.07.004.
49.- Urquiaga-Vargas TM. "Humanize to heal" as a care strategy in the Cardiological Intensive Care Unit of a specialized pediatric institute in Peru. Investig Innov Clin Quir Pediatr [Internet]. 23 April 2024 [cited 27 May 2024]; 2(1):76-8. Available in: https://investigacionpediatrica.insnsb.gob.pe/index.php/iicqp/article/view/85.
50.- Mir-Tabar A, Pardo-Herrera A, Goni-Blanco, et al. Satisfacción de los pacientes con los cuidados enfermeros en una Unidad de Cuidados Intensivos medida a través de la escala Nursing Inten-sive-Care Satisfaction-Scale (NICSS), Enfermería Intensiva, https://doi.org/10.1016/j.enfi.2023.10.004.
51.- Szymkowicz E, Bodet-Contentin L, Marechal Y, Ehrmann S. Comparison of communication interfaces for mechanically ventilated patients in intensive care. Intensive and Critical Care Nursing. 2024; 80: 103562. https://doi.org/10.1016/j.iccn.2023.103562.
52.- Nazari-Ostad, Z., Namazinia, M., Hajiabadi, F. et al. Efecto de las visitas familiares basadas en protocolos sobre los indicadores fisiológicos en pacientes de la UCI: un ensayo controlado aleatorizado. BMC Anesthesiol 24 , 18 (2024). https://doi.org/10.1186/s12871-023-02396-3.
53.- Indregard AR, Nussle HM, Hagen M, Vandvik PO, Tesli M, Gather J, Kunøe N. Open-door policy versus treatment-as-usual in urban psychiatric inpatient wards: a pragmatic, randomised controlled, non-inferiority trial in Norway. Lancet Psychiatry. 2024 May;11(5):330-338. doi: 10.1016/S2215-0366(24)00039-7.
54.- Petrinec AB, Wilk C, Hughes JW, Zullo MD, George RL. Self-Care Mental Health App Intervention for Post-Intensive Care Syndrome-Family: A Randomized Pilot Study. Am J Crit Care. 2023 Nov 1;32(6):440-448. doi: 10.4037/ajcc2023800.
55.- Shorofi SA, Dadashian P, Arbon P, Moosazadeh M. The efficacy of earplugs and eye masks for delirium severity and sleep quality in patients undergoing coronary artery bypass grafting in cardiac intensive care units: A single-blind, randomised controlled trial. Aust Crit Care. 2024 Jan;37(1):74-83. doi: 10.1016/j.aucc.2023.08.003.
56.- Pattison N, O'Gara G, Thomas K, Wigmore T, Dyer J. An aromatherapy massage intervention on sleep in the ICU: Arandomized controlled feasibility study. Nurs Crit Care. 2024;29:14–21. https://doi.org/10.1111/nicc.12957.
57.- van der Wal LI, Grim CCA, Del Prado MR, van Westerloo DJ, Schultz MJ, Helmerhorst HJF, de Vries MC, de Jonge E; ICONIC Investigators. Perspectives of ICU Patients on Deferred Consent in the Context of Post-ICU Quality of Life: A Substudy of a Randomized Clinical Trial. Crit Care Med. 2024 May 1;52(5):694-703. doi: 10.1097/CCM.0000000000006184.
58.- Quigley, N., Binnie, A., Baig, N. et al. Modelado del aumento potencial de participantes elegibles en ensayos clínicos con la inclusión de pacientes de la unidad de cuidados intensivos de la comunidad en Alberta, Canadá: un análisis de árbol de decisiones. Can J Anesth/J Can Anesth 71 , 390–399 (2024). https://doi.org/10.1007/s12630-023-02669-y.
59.- Gonçalves GH, Gazola M, Batista NT, Farinha FT, Souza JA, Razera AP, et al. Percepção de mães sobre a visitação aberta na unidade de terapia intensiva neonatal. Enferm Foco. 2024;15:e-202403.
60.- González MA, Alfie J. Una revisión acerca del cuidado de la salud mental en las familias de la Unidad de Cuidados Intensivos Neonatales. Rev. Hosp. Ital. B.Aires [Internet]. 29 de septiembre de 2023 [citado 28 de julio de 2024];43(3):p. 134-138. Disponible en: //ojs.hospitalitaliano.org.ar/index.php/revistahi/article/view/270
61.- Silva, J. D. S., Almeida, V. C., & Corrêa, E. A. (2023). O mundo privado na UTI: Análise da internação de pacientes oncológicos. Psicologia: Ciência e Profissão, 43, 1-12. https://10.1590/1982-3703003255152.
62.- Matos Júnior JM de, Pinheiro A de S, Reis DST dos, Borges WD, Sonobe HM, Correa Júnior AJS. Palliative care of nursing in the pandemic scenario according to the pacific end-of-life theory / Cuidados paliativos da enfermagem no cenário pandêmico conforme a teoria de final de vida pacífico. Rev. Pesqui. (Univ. Fed. Estado Rio J., Online) [Internet]. 30º de junho de 2023 [citado 28º de julho de 2024];15:e-12037. Disponível em: https://seer.unirio.br/cuidadofundamental/article/view/12037
63.- Moreno, Omar David Ávila, José Luis Vergara Centeno, and Joicy Anabel Franco Coffré. "Un desafío sanitario en la gestión del servicio de medicina crítica de un hospital del Ecuador: Vivencias en la pandemia COVID-19." Boletín de Malariología y Salud Ambiental 62.1 (2022): 2-7.
64.- Mateo Rodríguez E, Puchades Gimeno F, Ezzeddine Angulo A, Asensio Samper J, Saiz Ruiz C, López Alarcón MD. Postintensive care syndrome in COVID-19. Unicentric pilot study. Med Clin (Barc). 2022 Oct 14;159(7):321-326. English, Spanish. doi: 10.1016/j.medcli.2021.11.014.
Received: May 19, 2024 / Accepted: September 30, 2024 / Published: December 15, 2024
Citation: Quiroga I, Carvajal C., Vera L., Calderón M., Bejarano J, Hidalgo J. Post-ICU Syndrome and the Importance of Humanization in Intensive Care. Bionatura Journal 2024; 1 (4) 9. http://dx.doi.org/10.70099/BJ/2024.01.04.9
Additional information Correspondence should be addressed to jahidalgoacosta@hotmail.com
Peer review information. Bionatura thanks anonymous reviewer(s) for their contribution to the peer review of this work using https://reviewerlocator.webofscience.com/
ISSN.3020-7886
All articles published by Bionatura Journal are made freely and permanently accessible online immediately upon publication, without subscription charges or registration barriers.
Publisher's Note: Bionatura Journal stays neutral concerning jurisdictional claims in published maps and institutional affiliations.
Copyright: © 2024 by the authors. They were submitted for possible open-access publication under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




